Our surgeons use leading edge technology to perform innovative bariatric, general and colorectal surgeries designed to help patients achieve a healthier life.
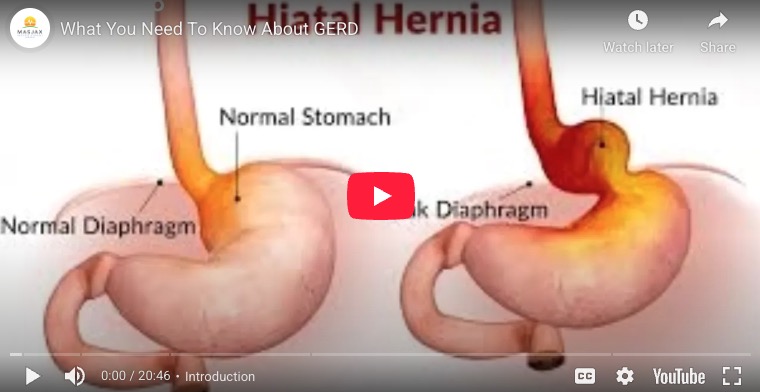
Bariatric Surgery Videos
Check out our video library to learn more about the bariatric journey.
View Video LibraryMeet Our Team
Our surgical program has a dedicated team to follow you every step of the way. Your multi-disciplinary team includes surgeons, (bariatric) nurses, dietitians, mental health professionals, exercise specialists, bariatric advocates and other medical specialists who offer continuous compassionate support and guidance in a respectful environment.
The focus is to help each patient establish and achieve their goals.
latest blog
Fiber Maxxing: Safe Weight Loss or A Potentially Unhealthy TikTok Trend?

Does “fiber maxxing” make sense, or is it just another viral, and possibly dangerous trend?
It is truly extraordinary to see the degree to which social media influencers and those looking to break into the influencer field will go to make a splash. Unfortunately, the result has been a significant increase in misinformation and unfortunate advice that has caused some to follow diets and exercise programs that don’t work and can, in some cases, lead to disordered eating.
With that said, there is a viral trend that has some legs, known as fiber maxing. Some even call it “Natural Ozempic.”
Some TikTokers claim to consume dozens of grams of fiber per day. Fiber is incredibly healthy – it fills you up, causing you to eat less, and it works wonders for GI and colonic health. However, there are also significant downsides to consuming too much fiber, especially when not accompanied by proper hydration.
So, to that end, let’s talk about fiber and any critical caveats of consuming fiber for weight loss. We’ll see if it makes sense, landing finally on what you should and shouldn’t do. (more…)