Nissen Fundoplication to Treat GERD
The Nissen Fundoplication has, over the past few decades, been considered the gold standard in surgical treatment for the symptoms of gastroesophageal reflux disease, or GERD. Typically, a fundoplication is indicated when the patient has not responded to conservative measures, such as lifestyle changes and medication, when they do not qualify for the LINX Reflux Management System, or when they have a paraesophageal hiatal hernia.
How a Fundoplication Works
Today, fundoplications are performed in a minimally invasive manner, meaning that four or five small incisions are made in the abdomen, versus the single large incision of traditional open surgery. The laparoscopic approach offers the same excellent, long-term symptom improvement, while minimizing many of the complications of a large single incision.
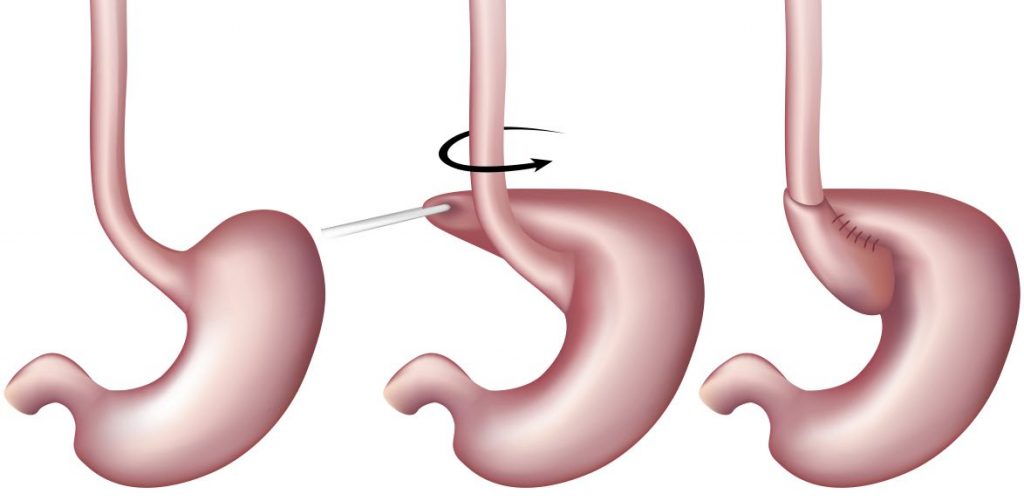
During the procedure, the upper portion of the stomach, known as the fundus is wrapped around the lower part of the esophagus. The stomach is then sutured in place for a permanent repair. This results in added pressure to the lower esophageal sphincter or LES, stopping corrosive stomach acid from refluxing back into the esophagus. If a hiatal hernia is present, this will be repaired during the primary fundoplication procedure.
In all, the fundoplication requires about 45-to-60 minutes of operative time under general anesthesia in a hospital setting. Most patients will spend one night in the hospital for observation. Once home, patients will be on a modified diet for about 4 weeks to allow the stomach to heal from the procedure.
Types of Fundoplications
When it was first invented, the fundoplication consisted of a total, or 360°, wrap around the esophagus. This was known as a Nissen Fundoplication. Because of some of the risks and limitations associated with the total wrap, partial wrap modifications were developed more recently. These include the Toupet, offering 270° of coverage, as well as the Dor, offering 180 to 200° of coverage. When choosing the appropriate application, patient selection is key and this is where employing a skilled, experienced surgeon in anti-reflux surgery is very important.
Results of the Fundoplication
Fundoplications are typically very effective, with most patients achieving complete elimination of severe symptoms associated with GERD. With the improvements in minimally invasive technology, the rate of serious complications due to a fundoplication is very low.
Risks and Considerations of a Fundoplication
As with any major surgical procedure, there are risks of surgery including reactions anesthesia, pain, blood loss, infection, and, in very rare cases, death. These risks can be mitigated by employing a skilled surgeon with significant experience in the procedure.
There is a less than 10% chance that the fundoplication will fail, but when it does, typically the suture line breaks. The stomach will return to its normal shape, and the lower esophageal sphincter will lose the added pressure offered by the fundoplication. While this complication is usually not severe, symptoms of GERD will ultimately return.
Patients undergoing a fundoplication may experience gas bloat syndrome, an uncomfortable situation in which swallowed air becomes trapped in the stomach and the small intestine. Because of the added pressure on the LES, this gas cannot be eliminated by belching. Over time, this risk is reduced. Patients can minimize the chances of gas bloat syndrome by avoiding carbonated beverages and eating slowly.
While the LINX procedure/device is becoming very popular for reflux management, there is still a place for fundoplication. We encourage you to take the next step and schedule a consultation with one of our surgeons to learn more about which anti-reflux procedure is right for you.