The Ideal Gastric Sleeve Patient
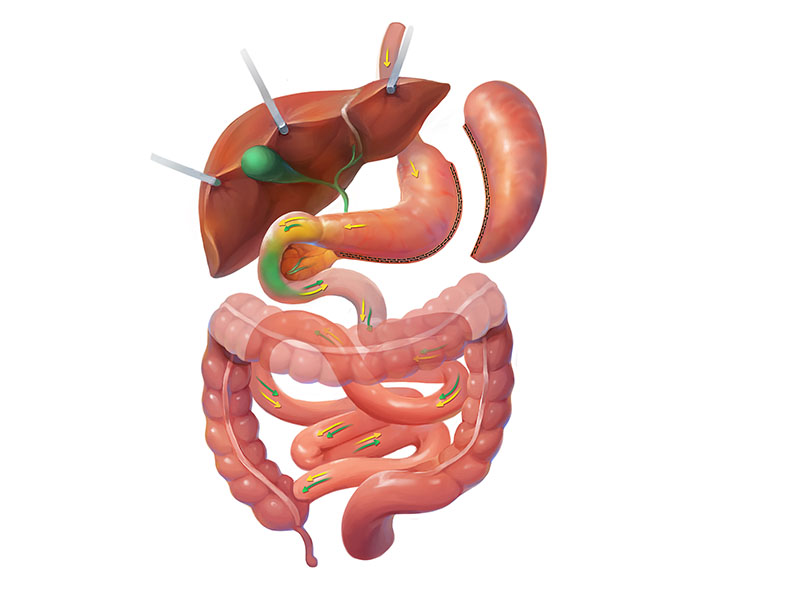
If you’ve researched bariatric surgery, you’ll notice several possible procedures to choose from. In fact, many procedures are available overseas that still need to be approved in the United States. However, the gastric sleeve is a tried-and-true procedure, ideal for many bariatric patients. To understand whether you are an ideal patient for gastric sleeve surgery, it’s best to watch our online seminar and schedule an appointment with one of our bariatric surgeons. In the meantime, you can use the following as a rough guide.
BMI: the gastric sleeve is typically best for patients on the lower end of the BMI qualification scale. Once patients cross into the 50 and 60 BMI range, a duodenal switch may be more appropriate.
Reflux: patients with significant acid reflux will be cautioned to avoid the gastric sleeve as it could worsen the condition. This is because the pressure within the gastric pouch increases after surgery. Typically, this pressure is released upwards rather than downwards, causing reflux. A gastric bypass generally is more appropriate in these patients.
Type 2 diabetes: patients suffering from poorly controlled or uncontrolled type 2 diabetes will likely see significant improvement with a gastric sleeve. However, gastric bypass truly is the gold standard for these patients. The gastric bypass often puts type two diabetes into remission within days of surgery, even before any significant weight loss has been achieved.
Cash Pay: for patients considering cash pay, the gastric sleeve is usually the most cost-effective procedure. Of course, the considerations above still apply, and we will not perform a sleeve on patients who are not good candidates. However, the cost of the sleeve can be up to half that of a bypass or duodenal switch.
Related Resources: